MedTech
Back Surgery Shifts to Preservation as New Procedure Gains Notice
Dong-A Ilbo |
Updated 2026.02.11
Relieving Nerve Compression While Preserving the Disc
Herniated Disc Gradually Shrinks as It Is Reabsorbed
Park Kyung-woo, CEO and Chief Director, Seoul Gwanghye Hospital
“Minimal Scarring Is Driving More Young Patients to Choose This Option”
Herniated Disc Gradually Shrinks as It Is Reabsorbed
Park Kyung-woo, CEO and Chief Director, Seoul Gwanghye Hospital
“Minimal Scarring Is Driving More Young Patients to Choose This Option”
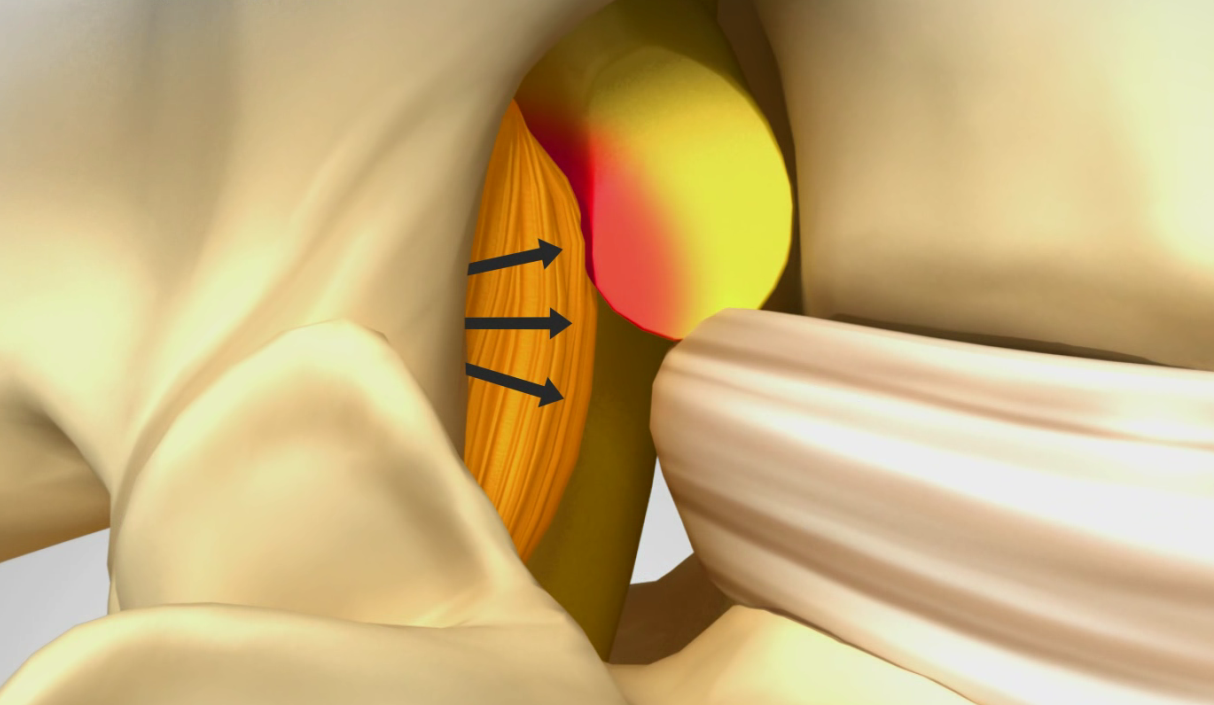
In the intervertebral foramen, the protruding disc at the front and the thickened ligamentum flavum at the back are compressing the nerve root.
Sharp, stabbing pain that shoots through the back when bending over or standing up suddenly after sitting for a long time is a familiar symptom for many people today. As the use of smartphones and laptops has become routine, lumbar disc herniation, commonly referred to as a herniated disc, is increasing rapidly even among younger people in their 20s to 40s. In the past, treatment focused on removing the herniated disc, but recently, techniques that preserve the disc while relieving nerve compression have emerged as alternatives. A representative method is “foraminal decompression.”The medical term for a herniated disc in the lower back is lumbar disc herniation. The intervertebral disc acts as a shock-absorbing cushion between vertebrae and consists of a central nucleus pulposus, the surrounding annulus fibrosus, and the endplates that contact the vertebrae above and below. When the annulus fibrosus weakens and the nucleus pulposus is pushed backward, it compresses the nerves, causing pain, numbness, and sensory disturbances.
The symptoms vary depending not only on the degree of disc herniation but also on the location and direction of the herniation. The lumbar spine consists of five segments, and when an upper segment is affected, pain is mainly felt in the central lower back. In contrast, the lower the affected segment, the more pronounced the radiating pain becomes, extending to the buttocks, thighs, calves, and toes. If the disc herniates toward the center of the spinal canal, symptoms may appear in both legs, whereas a herniation to one side leads to unilateral symptoms such as tingling in a specific leg. This is why patients with the same diagnosis of lumbar disc herniation can experience different patterns and intensities of pain.
Lumbar disc herniation often occurs together with spinal canal stenosis or foraminal stenosis. When the disc wears down and its height decreases, the space between vertebrae narrows, and the area of the intervertebral foramen—the passage through which nerves travel—also decreases. In this process, if the nerve root or dorsal root ganglion is compressed, the pain is more likely to become chronic.
In the early stages of lumbar disc herniation, symptoms often improve with medication, injections, and physical therapy. However, when symptoms recur or nerve compression is severe, treatments that remove the disc or cauterize it using heat or electrical energy have traditionally been used. When the disc is almost completely lost, this can lead to spinal fusion surgery, in which a cage is inserted to fix the vertebrae. Nevertheless, the more the disc is removed, the more the spine’s cushioning function decreases, and over the long term, the burden on adjacent segments can increase, a limitation that has been frequently pointed out.
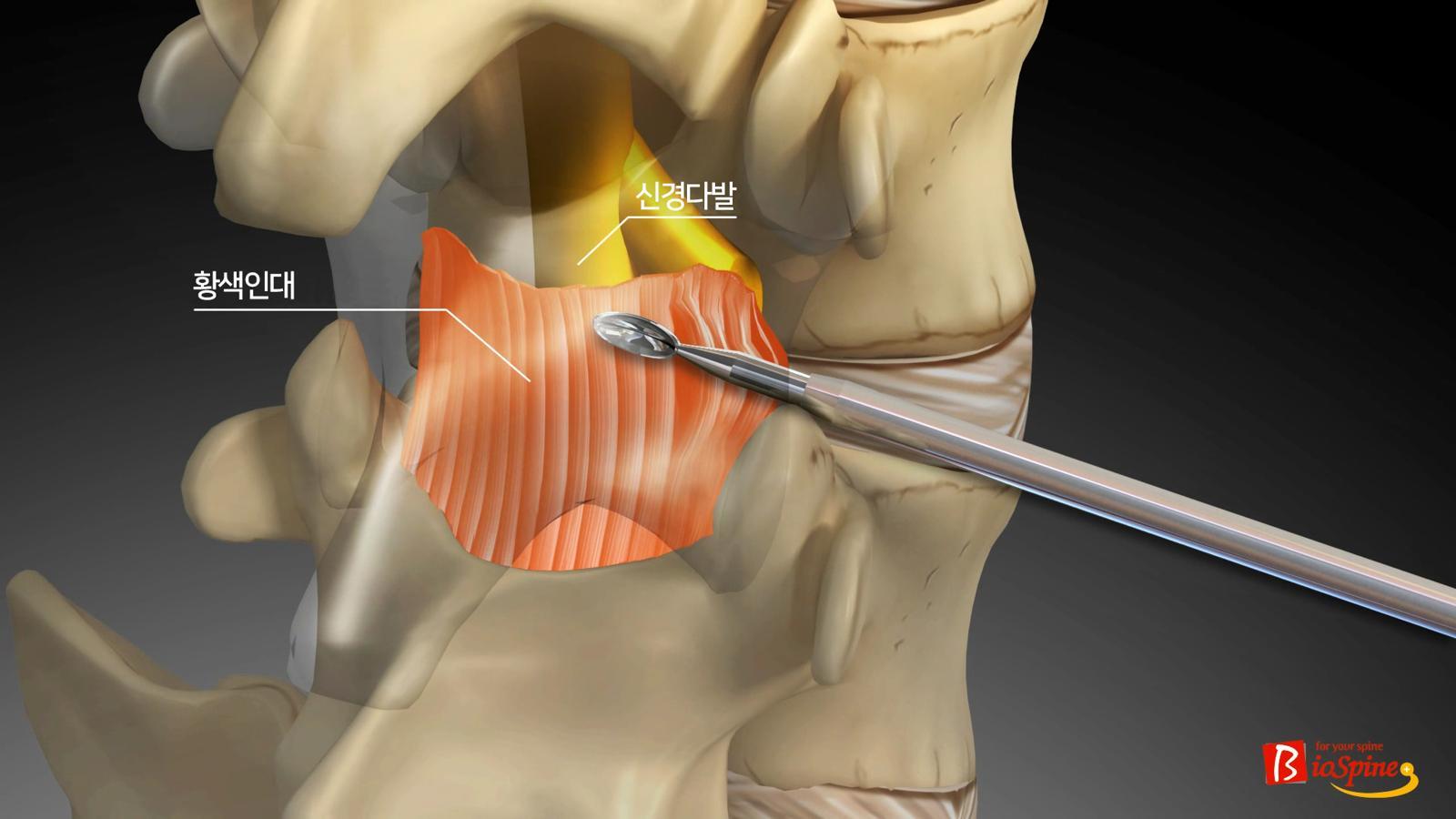
Foraminal decompression, in which a special kit is used to resect the ligamentum flavum at the posterior portion of the intervertebral foramen to widen the space. Seoul Gwanghye Hospital
Against this backdrop, foraminal decompression is attracting attention. This procedure focuses on relieving compression by widening the space of the intervertebral foramen, the passage through which nerves run, without directly removing the herniated disc. Based on the fact that the disc primarily compresses the nerve from the front, surgeons approach from the relatively safer posterior route and selectively remove the surrounding ligaments and ligamentum flavum around the foramen using specialized instruments. Compared with an anterior approach, where major blood vessels and nerves are concentrated, this method is assessed to carry a lower risk of complications.The most notable feature of this procedure is that the disc is left intact. Over time, a herniated disc can be naturally resorbed by the body’s immune response, a process known as “spontaneous resorption.” If nerve compression is alleviated early on to reduce pain, the herniated disc can gradually decrease in size. Since the disc is tissue that undergoes degenerative changes relatively quickly, artificial removal can actually accelerate degeneration, making this conservative approach particularly meaningful.
Park Kyung-woo, Chief Director of Seoul Gwanghye Hospital, said, “The paradigm of lumbar disc treatment is shifting from ‘how much of the herniated disc should be removed’ to ‘how to preserve the disc while controlling pain.’” He added, “The younger the patient, the longer the period during which they may be exposed to degenerative changes in the spine in the future, so it is essential to carefully evaluate the disc condition and degree of nerve compression to determine whether conservative treatment is possible. Foraminal decompression involves minimal incision, resulting in less muscle loss and scarring while preserving the disc, making it a treatment option that can be considered even for younger patients.”
Choi Hae-jin
AI-translated with ChatGPT. Provided as is; original Korean text prevails.
ⓒ dongA.com. All rights reserved. Reproduction, redistribution, or use for AI training prohibited.
Popular News