Medical / Research
Thin but Diabetic: Higher Mortality Risk
Dong-A Ilbo |
Updated 2026.01.14
Joint research team including Dongtan Sacred Heart Hospital
Tracking 1,788,996 type 2 diabetes patients… underweight linked to up to 3.8 times higher mortality risk
Higher cardiovascular and cerebrovascular mortality… possible malnutrition and muscle loss
Smoking cessation and balanced diet and exercise are essential
Tracking 1,788,996 type 2 diabetes patients… underweight linked to up to 3.8 times higher mortality risk
Higher cardiovascular and cerebrovascular mortality… possible malnutrition and muscle loss
Smoking cessation and balanced diet and exercise are essential
Lean diabetes is also dangerous
The problem lies in the opposite-direction risk of being “underweight.” A joint research team led by Professors Hong Eun-kyung and Choi Hoon-ji of the Division of Endocrinology and Metabolism at Hallym University Dongtan Sacred Heart Hospital, Professor Moon Sun-joon of the Division of Endocrinology and Metabolism at Kangbuk Samsung Hospital, and Professor Han Kyung-do of the Department of Information Statistics and Actuarial Science at Soongsil University conducted a nationwide retrospective cohort study. Using National Health Insurance Service data, they tracked 1,788,996 type 2 diabetes patients aged 40 or older who underwent health checkups between 2015 and 2016, following them through 2022. The team categorized underweight by body mass index (BMI) into three levels (mild: 17.0–18.4 kg/㎡, moderate: 16.0–16.9 kg/㎡, severe:
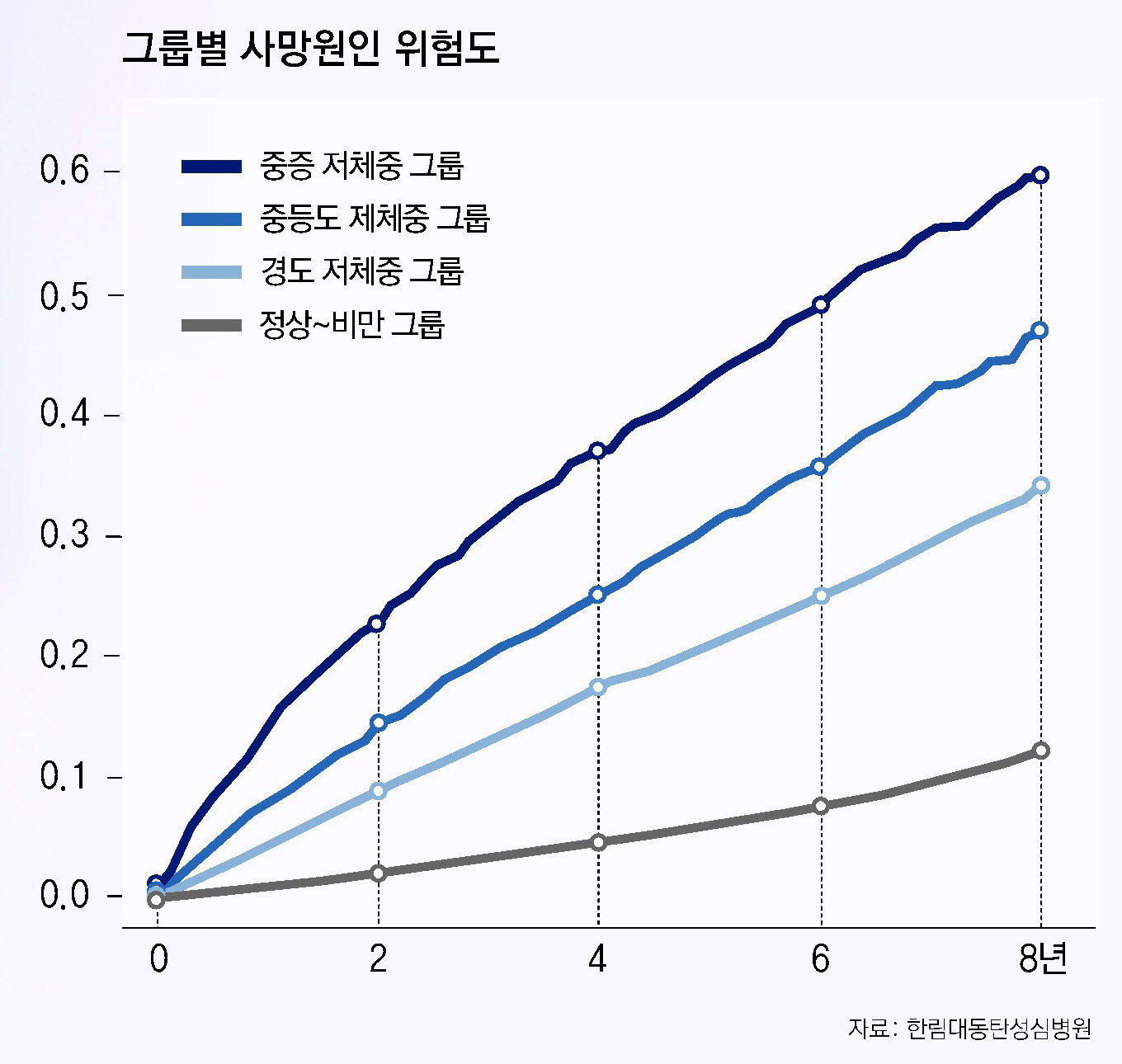
The results were straightforward. The mortality risk in the underweight group was up to 3.8 times higher than in the non-underweight group (normal to severe obesity). Mild underweight was associated with a twofold increase, moderate underweight with a 2.7-fold increase, and severe underweight with a 3.9-fold increase in risk, with lower BMI levels corresponding to higher risk. By cause of death, the underweight group had mortality rates 1.9–5.1 times higher from diabetes, cardiovascular disease, and cerebrovascular disease. Notably, underweight-related mortality risk was 6.2 among those under 65, higher than the 3.4 observed in those 65 and older. The adverse impact of underweight was thus greater in younger diabetes patients.
Symptoms of type 2 diabetes may not be pronounced in the early stages. Typical signs include increased thirst and frequent drinking of water, increased urine output (polyuria), weight loss despite increased appetite, and easy fatigability. Wounds may heal poorly, vision may feel blurred, and neurological symptoms such as tingling in the hands and feet can occur. Even if symptoms are vague or absent, elevated fasting blood glucose detected in a health checkup requires further evaluation.
Diagnosis is made through blood glucose testing. Fasting plasma glucose tests, glycated hemoglobin (HbA1c) tests, and, when necessary, 75 g oral glucose tolerance tests are used to determine the presence and severity of diabetes. After diagnosis, the risk of complications is assessed concurrently. This includes blood pressure and lipid (cholesterol) testing, kidney function tests (serum creatinine, urine albumin, etc.), ophthalmologic examinations, and evaluation of peripheral nerves and foot condition. Diabetes is not solely a blood glucose problem; it is a chronic disease that raises overall risks to blood vessels and organs.
The focus of treatment: blood glucose and body composition
The fundamental goal of type 2 diabetes treatment is to maintain blood glucose within an appropriate range to reduce the risk of complications. Treatment proceeds by combining lifestyle modification with pharmacotherapy. Dietary control and exercise are central, and oral hypoglycemic agents or injectables (including insulin) are used as needed. Medication choice is based on an overall assessment of the patient’s blood glucose level, disease duration, comorbidities (such as cardiovascular or kidney disease), hypoglycemia risk, and weight status.
In this study, underweight patients were more likely to be older, current smokers, and low income. They were also less likely to exercise regularly. Even after adjusting for variables such as age, sex, income level, lifestyle habits, fasting blood glucose, and diabetes duration, mortality risk in the underweight group remained higher than in the obese group. Taking the mortality risk of mild obesity as 1.0, the risks were 5.2 times higher for severe underweight, 3.6 times higher for moderate underweight, and 2.7 times higher for mild underweight, with all underweight groups having higher risk than the severe obesity group (1.5 times). This large-scale analysis indicates that underweight can be a critical risk factor for survival in diabetes patients.
Professor Hong Eun-kyung stated, “Underweight diabetes patients are more likely to be in a state of relative malnutrition or muscle loss, which can adversely affect survival rates,” and advised, “Rather than pursuing excessive weight loss for blood glucose control, patients should focus on maintaining overall nutritional balance and managing body composition in a well-balanced manner.” Given that lean diabetes is relatively more prevalent among Asians, some experts argue that BMI criteria for diabetes patients should be reevaluated not only from an obesity prevention standpoint but from the perspective of minimizing mortality risk.
Key precautions are clear. First, it is dangerous to conclude “I am far from diabetes” simply because body weight is low. Second, for those already diagnosed with diabetes, excessive weight loss under the notion that “I just need to lose weight” should be avoided. In particular, if a patient is underweight or has recently lost weight rapidly, nutritional status, muscle mass, and comorbidities should all be evaluated together. Third, as smoking increases the risk of vascular complications, smoking cessation is essential. Fourth, when using medications with a risk of hypoglycemia, skipping meals or engaging in excessive exercise can be dangerous and must be coordinated with healthcare professionals.
The direction of lifestyle modification also changes. While weight loss may benefit obese patients, for those who are underweight or have reduced muscle mass, the goal should be “maintenance and recovery” rather than “reduction.” A strategy is required that ensures adequate intake of protein and energy through a balanced diet and preserves muscle mass through resistance training. Aerobic exercise helps improve blood glucose, but for underweight patients, it is more important to complement body composition by combining it with strength training. Above all, the foundation of diabetes treatment is comprehensive management through regular testing not only of blood glucose but also of blood pressure, lipids, kidney function, eyes, and nerves.
Lean diabetes is not a mild condition. Reducing the risks of type 2 diabetes requires shifting from treatment that targets weight as a single number to management that addresses blood glucose, nutrition, and muscle together.
Hong Eun-sim
AI-translated with ChatGPT. Provided as is; original Korean text prevails.
ⓒ dongA.com. All rights reserved. Reproduction, redistribution, or use for AI training prohibited.
Popular News