Clinical Case
“Even With Uterine, Ovarian Cancer, Pregnancy Still Possible”
Dong-A Ilbo |
Updated 2025.12.20
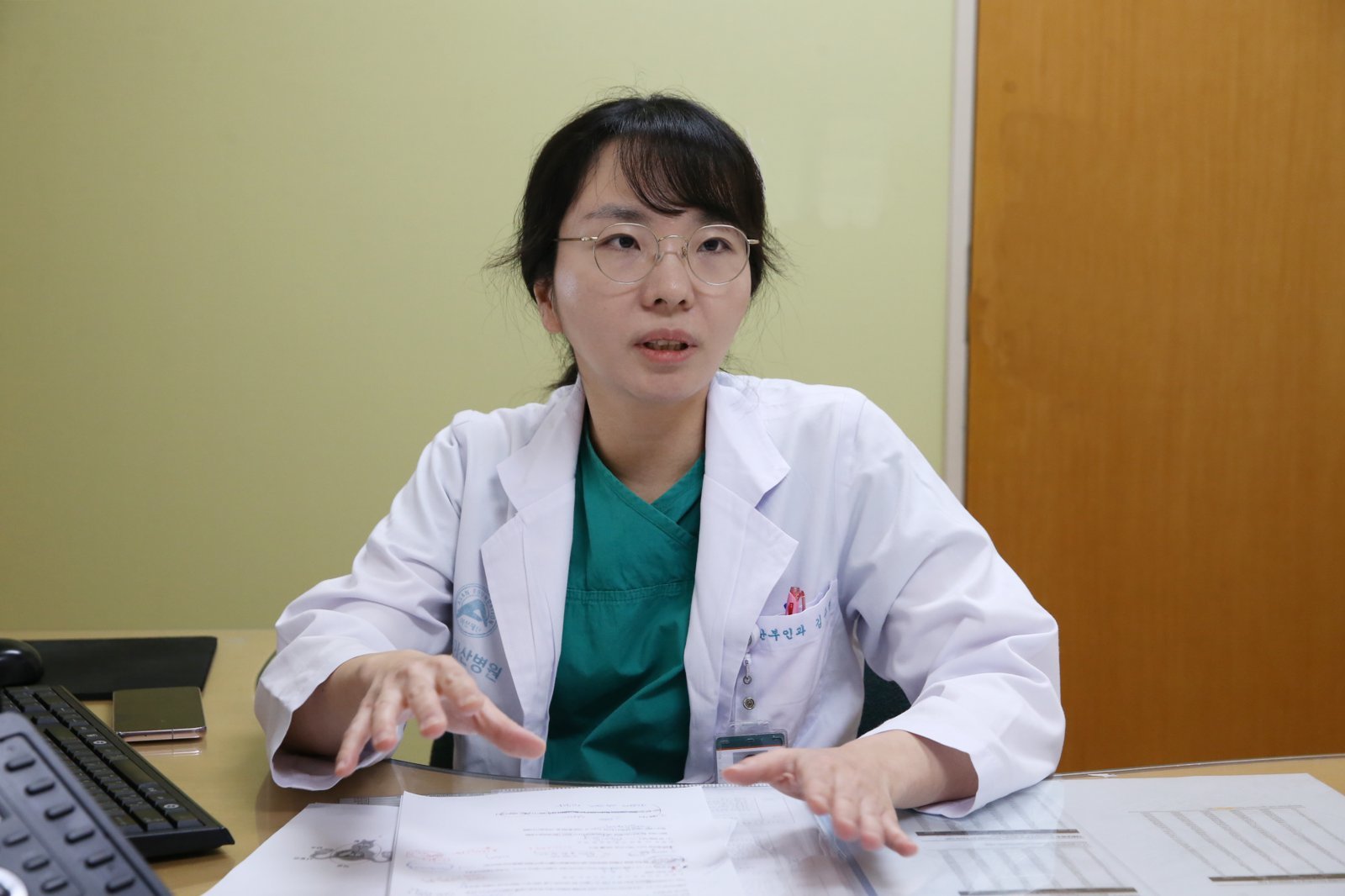
Prof. Kim Juhyun, Department of Obstetrics and Gynecology, Asan Medical Center, Seoul
Recent rise in gynecologic cancers among women aged 15–34
Standard surgery removes all reproductive organs… High cure rates but loss of fertility
Women in their 20s–30s who wish to have children
If stage I with low aggressiveness and other criteria met, uterine and ovarian function can be preserved for pregnancy
Patient determination and communication with physicians are crucial
Recent rise in gynecologic cancers among women aged 15–34
Standard surgery removes all reproductive organs… High cure rates but loss of fertility
Women in their 20s–30s who wish to have children
If stage I with low aggressiveness and other criteria met, uterine and ovarian function can be preserved for pregnancy
Patient determination and communication with physicians are crucial
Kim Joo-hyun, professor of obstetrics and gynecology at Asan Medical Center in Seoul, said that in young gynecologic cancer patients, if the cancer is at Stage I and has low aggressiveness, it is possible to preserve fertility and avoid removing the uterus and ovaries. However, she added that other necessary conditions vary by cancer type, so doctors and patients must communicate sufficiently to decide on treatment. Provided by Asan Medical Center
Cancers that occur in female reproductive organs such as the uterus and ovaries are called gynecologic cancers. The main types are cervical cancer, which develops in the cervix at the opening of the uterus; endometrial cancer, which arises in the inner lining of the uterine body; and ovarian cancer, which occurs in the ovaries on both sides of the uterus.As a “general rule,” when diagnosed with gynecologic cancer, both the uterus and ovaries are removed. If the cancer is detected at Stage I and surgery is performed, the five-year survival rate is up to 95%. However, future pregnancy becomes impossible. For young women who plan to give birth, this is a devastating blow.
Must the uterus and ovaries always be removed in gynecologic cancer? Does it mean pregnancy will never be possible again? Not necessarily. Professor Kim Joo-hyun of the Department of Obstetrics and Gynecology at Asan Medical Center in Seoul said, “In young patients with gynecologic cancer, the focus is not only on eradicating the cancer but also on preserving fertility so that pregnancy and childbirth remain possible. When conditions are right and treatment goes well, many patients are able to achieve both goals.”
● Rise in gynecologic cancers among young women, with obesity a major factor
Recently, the number of “young gynecologic cancer” patients has been increasing. According to the National Cancer Registry Statistics (2022), the three most common cancers among women in Korea are breast cancer, thyroid cancer, and colorectal cancer. Cervical cancer ranks eighth and ovarian cancer ninth. However, when limited to women aged 15–34, cervical cancer jumps to fourth and ovarian cancer to fifth, indicating a high prevalence of gynecologic cancers among young women. Professor Kim explained, “Obesity and Westernized dietary habits are the common underlying causes of the rise in gynecologic cancers among young women.” That said, the specific reasons for the increase vary somewhat by cancer type.
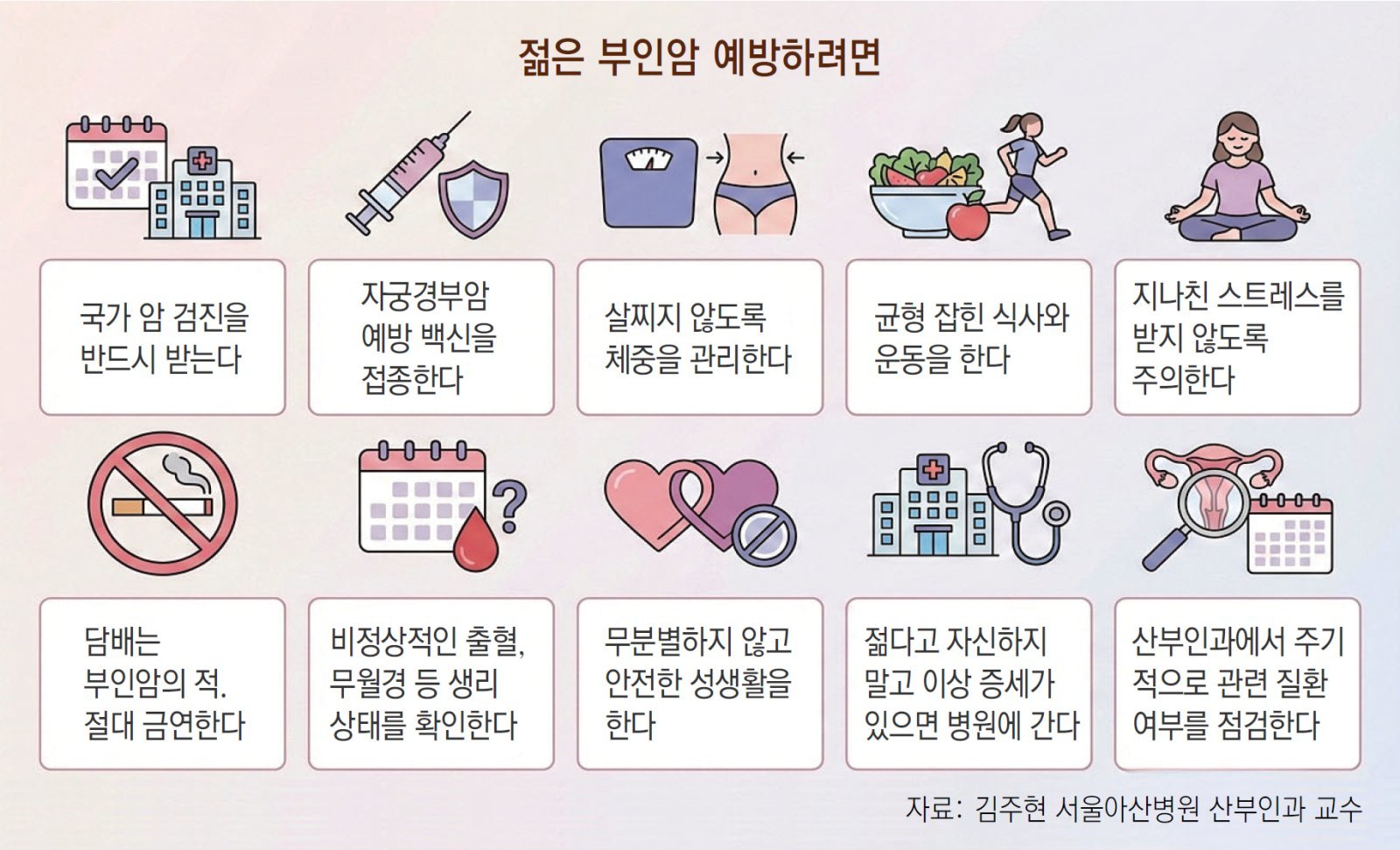
Cervical cancer is caused by infection with human papillomavirus (HPV). As more women receive vaccinations and the government implements free cervical cancer screening, the upward trend has leveled off. Nonetheless, there is criticism that the increase in cases among women in their 20s is due to many young women avoiding screening. Professor Kim said, “If women undergo screening, cervical cancer can be detected at a pre-cancerous stage, but the participation rate in national screening is less than 60%.” Cervical cancer is also closely related to sexual activity. The trend toward earlier onset of sexual activity compared with the past is another factor behind the increase in young cervical cancer patients.
Endometrial cancer is the gynecologic cancer that has been increasing most steadily. Professor Kim said, “It is related to the social climate in which women do not marry and have children, or delay childbirth.” During pregnancy, the placenta secretes a hormone called progesterone, which prevents excessive proliferation of endometrial cells. As a result, the risk of cancer decreases, but when women do not become pregnant, they remain fully exposed to this risk. In fact, many studies have found that pregnancy reduces the risk of endometrial cancer.
Ovarian cancer typically occurs after menopause, and in such cases, epithelial ovarian cancer accounts for the majority. In women in their 20s and 30s, however, germ cell tumors or borderline ovarian tumors are more common. These types generally respond better to treatment than epithelial ovarian cancer, making early detection important.
Pregnancy reduces not only endometrial cancer risk but also ovarian cancer risk. Frequent ovulation damages the epithelial cells of the ovary, and the accumulation of such damage can lead to ovarian cancer. During pregnancy, ovulation does not occur, allowing the ovaries to rest and thereby reducing cancer risk.
● Detecting early warning signs of cancer
In her mid-20s, a woman identified as Park Mi-hyun (pseudonym) experienced amenorrhea (absence of menstruation) for some time. Rather than being concerned, she felt it was convenient not to have periods. While accompanying a friend to the hospital, she unexpectedly underwent a uterine examination and was diagnosed with endometrial cancer.
Park did not intend to marry and identified as a non-marriage advocate. She had no plans for childbirth and opted for a hysterectomy. Even so, had she visited the hospital earlier, her cancer might have been detected at a pre-cancerous stage and her uterus preserved. Professor Kim said, “Regardless of age, how quickly cancer is detected has a major impact on treatment outcomes.” It is therefore important to recognize cancer symptoms. Although early-stage cancer may show no symptoms, careful observation can enable detection.
The most frequent symptom of cervical and endometrial cancer is abnormal bleeding. There may be bleeding outside of the menstrual period or post-coital bleeding. In some cases, as with Park, menstruation may cease altogether. Vaginal discharge mixed with blood may occur. Abdominal pain can also develop, particularly in the lower abdomen and pelvic area. When pain is present, there is a high probability that the cancer is already advanced.
Compared with other cancers, ovarian cancer is particularly difficult to detect early because it has virtually no initial symptoms. Professor Kim said, “Whether ovarian cancer is detected at an early stage is the key to successful treatment. At present, the best approach is regular monitoring, including health checkups.”
● Conditions for fertility-preserving treatment
Even in cases of gynecologic cancer, if fertility can be preserved, future pregnancy and childbirth are possible. However, fertility-preserving treatment cannot be applied to all patients. When it is deemed feasible, treatment is provided to eradicate the cancer while preserving the uterus and ovaries.
For cervical cancer, fertility-preserving treatment is possible only when the cancer is at Stage I, the tumor is smaller than 2 cm, and the aggressiveness is low. Various tests are conducted to determine eligibility. If the conditions are met, the cervix is removed and the uterine stump is sutured. Without suturing the stump, pregnancy cannot be maintained.
A woman in her mid-20s, identified as Lee Hye-sun (pseudonym), underwent this surgery after being diagnosed with cervical cancer. Her first attempt at pregnancy failed, but the second attempt was successful and she delivered a healthy baby. Lee is currently in good health and undergoing regular follow-up for cancer surveillance.
The conditions under which fertility-preserving treatment can be attempted in endometrial cancer are similar. The cancer must be at Stage I, confined to the endometrium, and have low aggressiveness. High-dose progesterone hormone therapy is administered. Initially, the outcome is checked at three-month intervals, and later at six-month intervals. If the cancer is not eliminated after a considerable treatment period, hysterectomy is considered.
A woman identified as Ko Min-seon (pseudonym), who was diagnosed with endometrial cancer in her early 30s, followed this course. She had an obese body type and first lost weight, then underwent six months of hormone therapy. She subsequently conceived and gave birth to twins.
Fertility-preserving treatment is also possible in ovarian cancer if the disease is at Stage I and both malignancy and aggressiveness are low. Additionally, the cancer must be confined to one ovary and not involve both. However, in cases of epithelial ovarian cancer, which is regarded as malignant, fertility-preserving treatment must be decided with particular caution.
● Challenges that remain
The complacent belief that “being young means being safe” is a major obstacle to cancer detection and treatment. Professor Kim said, “It is surprisingly common for young women to think they are not at an age where they can develop cancer, and therefore not to take symptoms seriously. In such cases, even when symptoms appear, valuable time is wasted.” Societal prejudice is another barrier. Professor Kim noted, “Many young women are reluctant to visit an obstetrician-gynecologist because of the perception that people will question why a young woman is going there, especially if she has no sexual or childbirth experience.”
There are also calls to improve the special copayment reduction system for young gynecologic cancer patients. Under this system, patients with cancer, severe disease, or rare conditions pay only 5–10% of medical costs for a set period (usually five years). Even if diagnosed with gynecologic cancer, patients are no longer eligible for benefits after five years. The problem is that gynecologic cancer patients who wish to preserve fertility require ongoing monitoring and treatment beyond five years. There are not a few cases in which treatment is abandoned or the uterus and ovaries are removed and pregnancy relinquished because treatment costs suddenly surge once the benefit period ends.
This was the case for a woman identified as Shin Mi-jin (pseudonym), who received treatment for endometrial cancer in her early 20s. The cancer disappeared within two years, but her medical follow-ups continued. When the special copayment reduction period ended, her medical expenses rose sharply. Shin stopped treatment, and a few years later, the cancer recurred. By then, it had progressed beyond Stage III, and her uterus had to be removed. Had she continued to receive the benefit, the recurrence could have been detected early and her uterus preserved. Professor Kim said, “I have seen many young gynecologic cancer patients who shoulder all aspects of treatment on their own. They need more support.”
Kim Sang-hoon
AI-translated with ChatGPT. Provided as is; original Korean text prevails.
ⓒ dongA.com. All rights reserved. Reproduction, redistribution, or use for AI training prohibited.
Popular News